Northern Colleges Provide Vital Cross-Training to Meet Departmental Demand
Health Sector article – 11/30
 For healthcare employers, the fast-moving field of nursing can feel like a particularly frustrating game of whack-a-mole.
For healthcare employers, the fast-moving field of nursing can feel like a particularly frustrating game of whack-a-mole.
Hire an extra hand to staff the ER, for example, and suddenly… there’s a shortage in surgical or obstetrics. That struggle for attrition, familiar to any hospital administrator, has only intensified in the wake of COVID-19. And because each environment presents such unique challenges and requires such specific training, it’s not like you can just “mix and match.”
Actually, it turns out you can.
In fact, with the benefit of a bit of career education, it turns out nurses can do pretty much anything.
“Our partnered transition-in-practice programs have gone a long way toward addressing immediate staffing needs to ensure adequate personnel are available to provide safe, high-quality patient care,” says Lawson Stuart, Director of Clinical Education and Professional Practice at Dignity Health of Sacramento. “The programs have afforded existing staff the opportunity to train into a new specialty field of interest.”
Dignity Health is just one of the industry partners collaborating with California Community Colleges to deliver these cross-training programs from Sacramento to Eureka. Bolstered by funding from the Health Workforce Initiative (HWI), the innovative effort represents a surgical approach to the persistent problem of specialty nursing shortages.
“Despite aggressive and costly recruiting efforts, it can still be very difficult to fill vacancies with experienced RNs in Labor & Delivery, Emergency Department, Surgery and the ICU,” says Stuart. “Developing local training programs has proven an effective solution.”
When it comes to nursing careers, versatility isn’t just a virtue – it’s vital. And while a nurse’s specialization may be defined by a particular alphabetical suffix, the letters don’t tend to spell out the entire résumé. So when the North Far North Regional Consortium and its partners began exploring ways to bridge critical cross-departmental skills gaps in nursing, it became a problem not driven by ability, but by access.
When Enloe Medical Center, for example, encountered an urgent need for Medical-Surgical nurses in Butte County, administrators had a choice to make. Rather than invest the time, money and effort into building an independent training program from the ground up, Enloe opted to take advantage of high-quality, expert-led courses from an already existing – and expanding — infrastructure.
Health care employers “can’t run a training program – it’s too expensive,” says Julie Holt, one of two Regional Directors of Employer Engagement tasked with leading the NFNRC’s response to the critical challenge. “So… how can we leverage these resources together?”
 The answer would lie in education. By applying the versatile skill sets of general nurses, for example, to subspecialties like ICU and obstetrics, a hospital could adapt to changes in demand without resorting to temporary hires or costly upskilling programs. For impacted departments, that agility translates to increased efficiency, better job security, and fewer instances of “burnout.” For the nurses themselves, it’s a step up professionally… and often in salary, as well.
The answer would lie in education. By applying the versatile skill sets of general nurses, for example, to subspecialties like ICU and obstetrics, a hospital could adapt to changes in demand without resorting to temporary hires or costly upskilling programs. For impacted departments, that agility translates to increased efficiency, better job security, and fewer instances of “burnout.” For the nurses themselves, it’s a step up professionally… and often in salary, as well.
“They usually get a raise,” says Trudy Old, Regional Director of Employer Engagement for the Far North. “If they want to specialize, they can take that course – then they become available for the hospitals to utilize them across [specialties].”
The programs, typically capped by two-day, intensive review courses, allow grads to test for the new specialization, opening the door to new opportunities and even a higher salary.
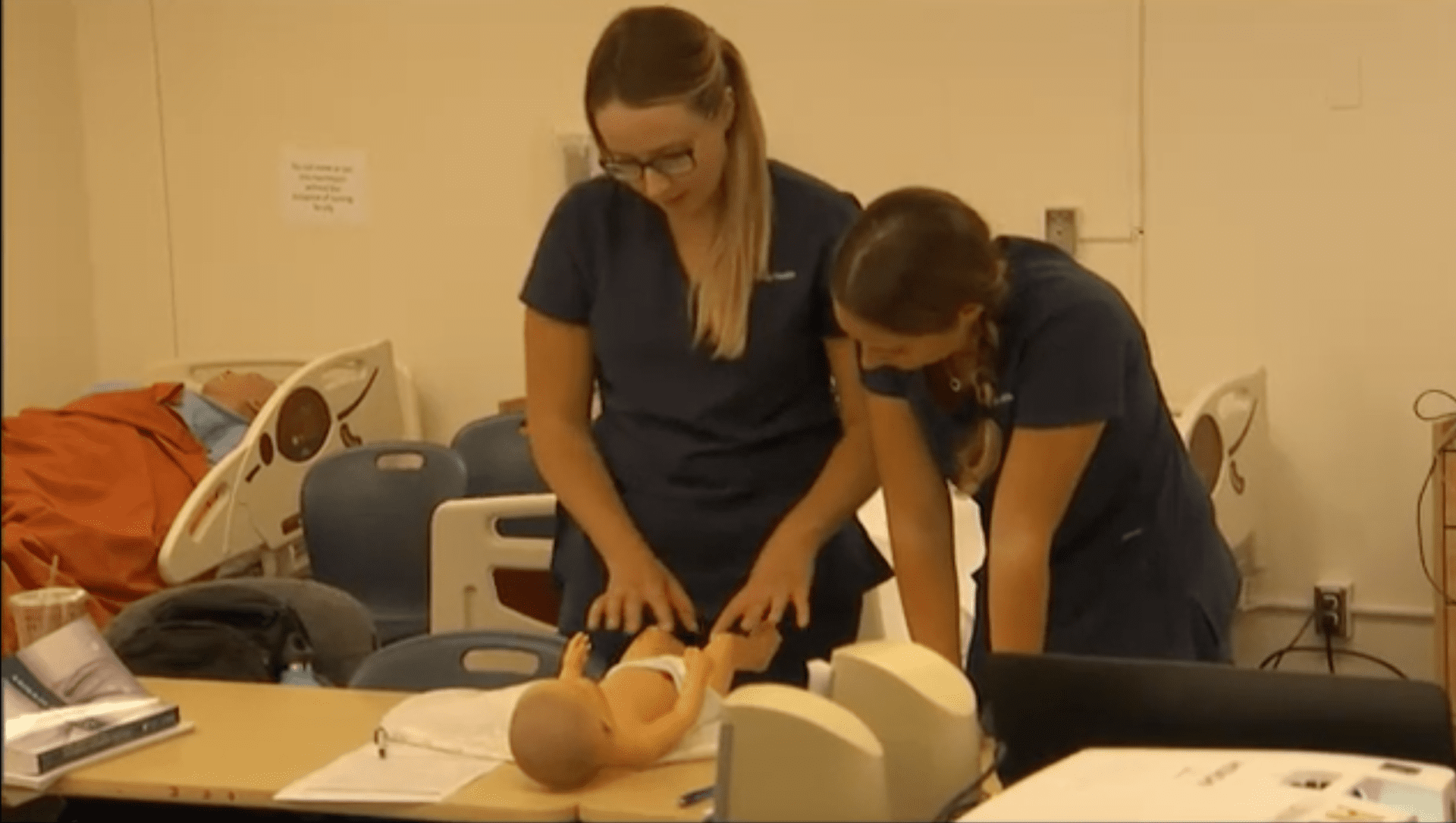
Last January, the NFNRC partnered with Enloe Medical Center in Chico to run two such programs – one for Med-Surg nurses and the other for Certified Pediatric Emergency Nursing (CPEN). Both workshops brought in students from as far away as Eureka, providing a much-needed opportunity to bolster nursing proficiencies in the Far North region.
The best part? It’s basically free of charge for upskilling nurses, who pay only the costs of course materials and lunch.
“The industry needs people specialized in these [areas] and don’t always have the training courses,”: says Old, who estimates that each course produces 30-60 new specialty nurses. “It can be really expensive when they charge it back to the students.
“Us being able to help them — it’s a win-win for the colleges and industry.”
Meanwhile, Holt and her health care industry contacts were busy strategizing in the North region, which includes the Greater Sacramento and Lake Tahoe areas. Building on the early success of transition-in-practice courses ongoing since 2018 with Sierra, American River and Sac City Colleges, the NFNRC continued to harness Strong Workforce Program funding to augment regional nurse preparedness.
The 4- to 6-week programs delivered critical cross-training to small cohorts of around 35 nurses at each participating college. Not only are the programs free to students — due to the dire skills gaps in sub-specialty positions, employers like Dignity Health often pay them to attend. It’s a double-win for the nurses, who learn their new specialization from the best teachers of all: industry-experienced nurses themselves.
“Expert clinicians are also expert educators,” says Holt, who credits the flexibility of partners on both the employer and education side for the program’s success so far. “I’ve worked hard as an RD to have these ongoing, honest evaluation conversations [and] faculty have been very willing to adapt to meet employer needs, based on relationships we’ve built over time.”
The success of the early programs at Enloe and Dignity inspired new incumbent worker training programs, in areas like Labor and Delivery, IV/Blood Withdrawal, and more. And though 2020 was expected to be the flashpoint for this new evolution in professional development, many of the partners’ existing plans were derailed by the COVID-19 crisis.
The irony, says Old, is that while the virus triggered mass furloughs through much of the state, the effects of the crisis will ultimately drive demand for specialized nurses up.
“Hospital beds weren’t full, and it cut into a lot of surgeries,” says the regional director. “I think COVID has caused some burnout. They’re taking on a lot of work, and burnout happens in all health fields. The fact is that some nurses will leave and retire.”
For health care providers like Dignity Health, the existence of a self-sustaining and always-improving pipeline translates to better patient care, now and into the future.
“Retaining long-tenured, experienced nursing staff who know and align with our mission and our ministry improves the patient experience overall,” says Stuart.